COTW: 3/14/22: 60 year old male with hoarseness
A 60 year old male with history of lung cancer presents to the ED with hoarseness. Patient is deaf and requires ASL. Patient also endorses sore throat and difficulty in breathing. Vital signs: BP 90/40, HR 120, RR 20, O2 94% RA, T 98.5. Physical exam: patient tachypneic, uncomfortable appearing and using accessory muscles to breath, patient is unable to lie supine. Airway patent without exudates or evidence of Ludwig’s, peritonsillar or retropharyngeal abscess. While waiting for ASL translation POCUS was used for evaluation.
Bedside ultrasound showed the following:
Large pericardial effusion in PLAX view.
Large pericardial effusion with evidence of RV free wall collapse. PSL view.
Pericardial Effusion/Tamponade
Common symptoms:
Exercise intolerance/dyspnea on exertion
Cough
Fatigue/shortness of breath
Pleuritic chest pain
Hiccups: phrenic nerve irritation/compression
Hoarseness!!!!
Recurrent laryngeal nerve compression
The left recurrent laryngeal nerve lies near the aorto-pulmonary window. Enlarged mediastinal lymph nodes (as well as inflammation pressing against the nodes) cause compression of such nerve and leads to hoarseness
Recurrent laryngeal nerve paralysis as a result of cardiovascular disease is also called “Ortner’s syndrome”
it results from the proximity of the heart and vessels
Pericardial effusion
Left atrial enlargement
Mitral stenosis
Penetratring aortic ulcer, patent ductus arteriosus (PAD), aortic aneurysm, giant cell arteritis
Left recurrent laryngeal 1.75X more common to be affected than the right
Physical Exam
Pulses paradoxus: 82% sensitive
Tachycardia: 77% sensitive
Tachypnea
Friction rub
Hypotension (narrow pulse pressure)
Muffled heart sounds
Causes:
Pericarditis
Uremia
Myopericarditis
Malignancy
Lung cancer, Hodgkin lymphoma, non-Hodgkin lymphoma, leukemia
Infections
Lupus
Hypothyroidism
Post-radiation: effusion may occur up to 20 years after therapy
Trauma
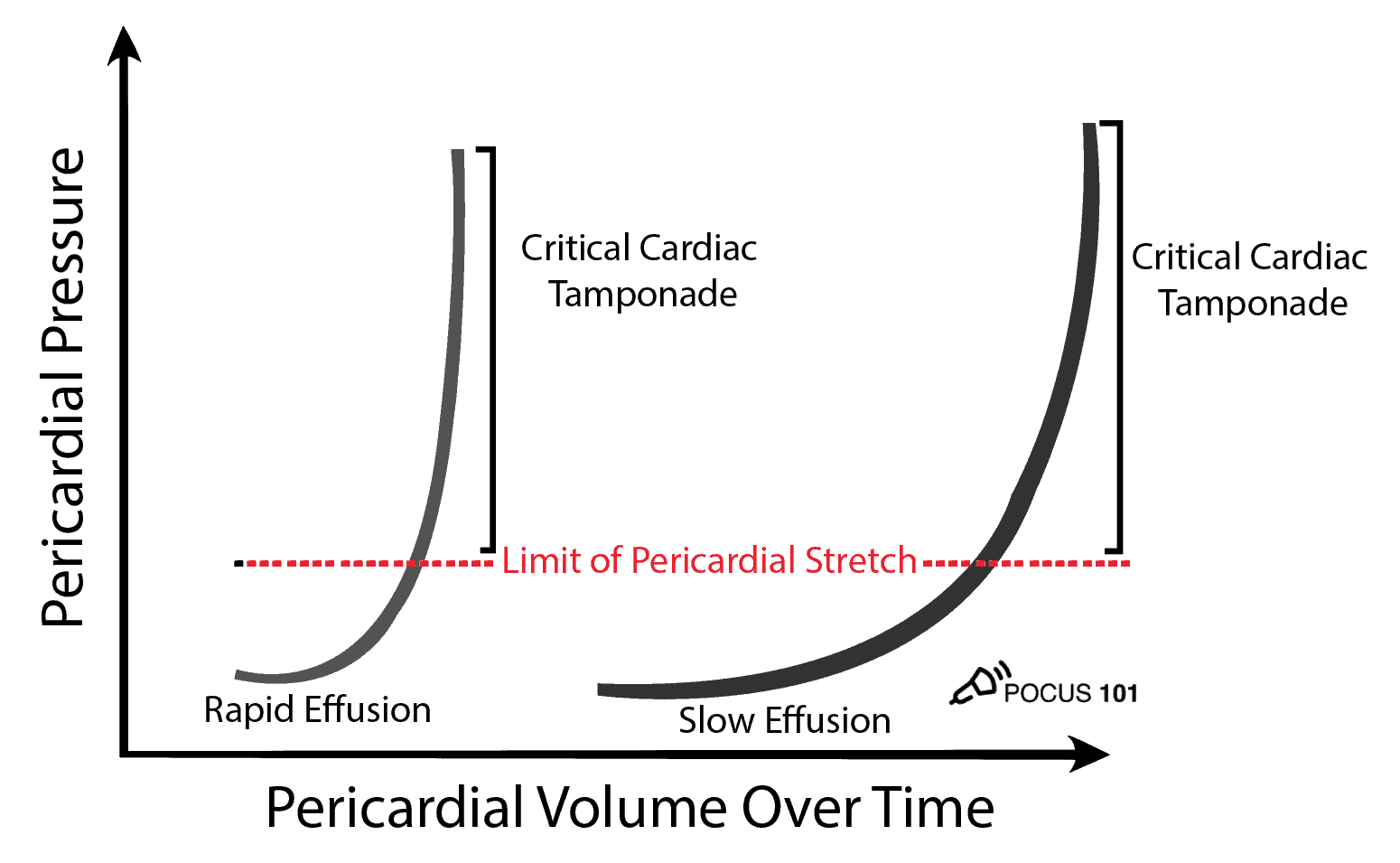
*** Reminder: It is not the size of the effusion, but the velocity that it accumulates that leads to cardiac tamponade. As little as 150-200mL of fluid can cause tamponade if the filling occurs quickly ***
*** The pericardial space is normally filled with <50 ml of fluid ***
Rapidly accumulating pericardial effusion can increase the pericardial pressures significantly and lead to tamponade.
Image Acquisition
Pericardial effusion is seen anterior to the descending aorta as portrayed in image. Pleural effusion is posterior to the descending aorta.
Work Up
CXR, CBC, Trop/BNP, coags, type and screen
EKG
Low voltage QRS
Electrical alternans
Non-specific ST/T wave changes
POCUS and Tamponade
Lower complication rate when compared to blind approach
0.5%-3.7 with ultrasound vs 15-20% blind
Allows operator to visualize real-time needle throughout the entire procedure
ECHO findings of Tamponade:
Pericardial effusion
Right atrial collapse during systole: earliest sign. Collapse lasts > 1/3 of cardiac cycle.
Right ventricular collapse during diastole: high specificity (75-90%)
Plethoric and non-variable IVC: high sensitivity (95-97%)
Mitral valve inflow decrease of >25% <———DR. ABRAMS SPECIAL!!!!!
Tricuspid valve inflow increase of >40%
Surrogate for pulsus paradoxus
*** Patients that have elevated right side pressures, diastolic collapse will less likely occur ***
Size:
Small < 1cm. Volume 50-100 ml
Moderate 1-2 cm. Volume 100-500 ml
Large >2cm. Volume > 500ml
***Pericardial fat pad: moves with heart during the cardiac cycle. Distributed in anterior atrioventricular groove***
Fat pad visualized anteriorly is iso-echoic versus pericardial effusion (anechoic).
Pericardiocentesis
Potential complications
Right ventricular puncture
Pneumothorax
Gastric puncture
Liver puncture
Hemorrhage
Ventricular arrhythmia
Pulmonary edema (pericardial decompression syndrome)
May develop few hours to days later. Occurs due to acute left ventricular overload secondary to persistent catecholaminergic peripheral vasoconstriction.
Contraindications
Aortic dissection
Free wall rupture
What do you need?…
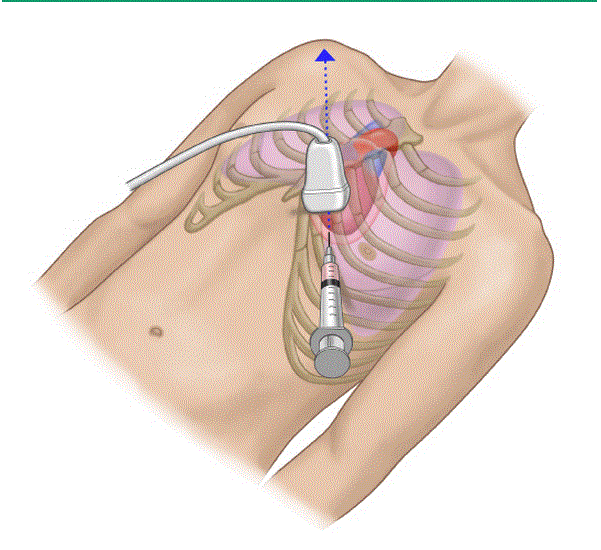
Approach
Subxiphoid
Highest complication rate
Potential structures to be damages: liver, lung, IVC, internal thoracic artery, left anterior descending aorta, colon and stomach
Longest distance from skin to pericardial fluid
Subxiphoid approach. Insert needle (not in plane) between xiphoid and left costal margin. Aim to left shoulder.
Parasternal
Shorter skin to pericardium distance
Complication: internal mammary artery (on lateral edge of sternum), pneumothorax
Limited in cardiac arrest
Parasternal approach. Insert needle in at/close to 5th left intercostal space. Needle in plane aiming to patient’s right shoulder.
Apical
Use high-frequency (linear) probe!!
Shortest skin to pericardium distance
Complication: pneumothorax, ventricular puncture
Apical approach: Introduce needle over the superior border of the adjacent rib to avoid intercostal nerves/vessels. Needle is introduced lateral to ribs 5-7. Aim towards the patient's right shoulder.
Pericardiocentesis: apical approach. Needle visualized top right of screen.
Apical approach using high-frequency probe. Needle visualized top right of screen.
Teaching Points
Rate of accumulation is predicting of tamponade rather than the size of effusion
Pericardiocentesis PLAX and apical approach have less complications when compared to SubX approach
Choose the site with the largest effusion closest to the probe
PLAX approach is favored but it is limited in cardiac arrest during cardiopulmonary resuscitation
Remember atypical presentations: hoarseness, hiccups